Claims management virtual assistant services are designed to streamline your claims process, reduce errors, and free up your internal team’s time. Stealth Agents provides skilled virtual assistants who handle everything from claim verification to compliance, helping you boost efficiency and focus on growth—get started today at
Managing claims efficiently can feel overwhelming, especially when accuracy and timeliness are crucial to your business operations. Hiring a claims management virtual assistant can save you hours of administrative work while ensuring every step, from filing to follow-ups, is handled with precision. Delays or errors in claims processing can result in lost revenue and frustrated clients, but there’s an easy solution to these common issues.
At Stealth Agents, we specialize in providing skilled virtual assistants who streamline claims management to reduce errors and improve your workflow. Whether it’s handling insurance claims or keeping communication with clients seamless, our team delivers reliable support tailored to your needs.
Studies show that businesses can cut operating costs by nearly 70% with virtual assistant services, leaving you with more resources to focus on growth.
Book a free consultation today to explore how we can help simplify claims management for your business.
What is a Claims Management Virtual Assistant?
A claims management virtual assistant helps businesses handle claims faster and more accurately by automating repetitive tasks like data entry and document processing.
These assistants reduce human error, saving companies time and money. Studies show that automation can lower administrative costs by up to 30%.
They can also analyze claims data to identify patterns, helping organizations make better decisions. By handling routine inquiries, they free up staff to focus on complex cases requiring human expertise.
Their use improves customer response time, enhancing satisfaction and trust.
What Tasks Can You Delegate to a Claims Management Virtual Assistant?
Managing claims can take up a huge chunk of your time, especially if you’re dealing with a lot of paperwork, follow-ups, or errors. A Claims Management Virtual Assistant can take over these tasks, freeing up your schedule and making your business run smoother.
Below, we’ve listed some of the most valuable tasks you can delegate, all of which can save you time, reduce stress, and improve accuracy.
1. Processing Insurance Claims
Your Claims Management Virtual Assistant can handle the tiring process of sorting, filing, and processing claim forms. This includes verifying documents, updating claim records, and following up with insurance providers. If you’ve been overwhelmed by delays, delegating this task can speed things up.
Having insurance claims virtual assistance ensures your claims are always on track and accurate. Reliable claim processing outsourcing can ease the stress of mistakes and help you avoid costly errors.
A virtual claims assistant ensures every claim is checked thoroughly, leaving no room for overlooked details. By having this support, you can focus on growing your business while your claims get handled efficiently.
2. Reviewing Medical Claims
Medical claims involve many specific terms, codes, and forms that require special attention. A medical claims virtual assistant can take over this tricky task and ensure that everything adds up.
They’ll review eligibility documents, catch errors that may delay payments, and ensure compliance with healthcare rules.
They claim knowledge as a virtual assistant can reduce costly mistakes, which is especially important with medical billing.
A bottleneck medical virtual assistant can reduce backlogs caused by claims piling up. Outsourcing this work ensures your medical claims are submitted on time and hassle-free.
With this support, your clinic or hospital can run like clockwork without worrying about filing errors.
3. Managing Billing and Payments
Keeping track of billing and payment deadlines is one of those stress-inducing tasks that is easy to mess up. A virtual billing assistant can stay on top of invoices, payment approvals, and reminders to ensure nothing is overlooked.
This is particularly beneficial if your practice processes multiple claims daily. Having insurance virtual assistants manage these tasks prevents revenue from slipping through the cracks. With their help, you can even reduce issues like late payments or missed invoices.
Your virtual claims management assistant will also handle any follow-ups for overdue payments, making your workday less stressful.
Delegating billing frees you up for more high-priority business decisions.
4. Detecting Insurance Claim Fraud
Insurance claim fraud is a sneaky problem that can cost you a lot if left unchecked. Delegating this task to a virtual claims assistant ensures fraudulent activities are caught early.
They can review claims for irregularities, check every detail, and identify anything that seems suspicious.
With insurance claim fraud detection being handled by a professional, you get an extra layer of security. This can protect your business from unnecessary payouts or legal troubles.
Having someone else handle this allows you to focus on legitimate claims and running your business. Knowing that all claims are rigorously checked for accuracy will give you peace of mind.
5. Updating Claim Records
Every claim must be logged, tracked, and updated to ensure smooth communication and proper resolutions. A virtual verifier assistant can keep your records organized and current.
This includes uploading claim updates, adjusting client details, and informing all relevant parties. Without accurate records, mistakes can creep in and delay claim closures. Insurance claims virtual assistance can save you hours by handling these updates quickly and correctly.
A well-maintained record system is essential for smooth workflows and faster claim approvals.
Delegating this responsibility means fewer headaches and better access to important data anytime you need it.
6. Communicating with Clients and Providers
Keeping clients informed about their insurance claims can be time-consuming, especially if they call with lots of questions. A virtual claims management assistant can handle these communications for you.
They can call clients, send updates, or answer questions about the status of claims. They’ll also work as a liaison between insurance providers to clarify details or request missing information. With their help, you’ll improve customer satisfaction without adding extra work to your plate.
The best medical claims virtual assistant knows how to handle tricky conversations with both professionalism and care. Delegating communication lets you focus on other core aspects of your business.
7. Auditing Claims for Errors
Errors in insurance claims can lead to rejected submissions and delays in payments. A virtual claims assistant can audit your claims and catch these issues before they become a bigger problem.
They’ll double-check documentation, ensure codes are correct, and flag any inconsistencies. By delegating this task, you can avoid costly resubmissions and processing delays.
Claiming knowledge from a virtual assistant means they stay up-to-date on requirements for error-free submissions.
This is key for industries like healthcare, where so much depends on accuracy and deadlines. You’ll enjoy smoother claim approvals and fewer back-and-forth corrections.
8. Coordinating with Insurance Providers
Negotiating with insurance providers can sometimes feel more complicated than it should. Your virtual claims assistant can take over this back-and-forth to ensure clear communication and faster resolutions.
They can handle disputes, clarify requirements, and arrange follow-ups with provider reps. This is particularly useful for businesses with busy workloads that can’t afford lengthy calls or emails.
With insurance virtual assistants managing negotiations, there’s no confusion or miscommunication. This support helps resolve issues more smoothly and gets claims moving forward without delays.
You’ll also expand your bandwidth for other projects when you’re not caught up in back-office negotiations.
9. Following Up on Pending Claims
It’s frustrating when claims stall, waiting for approval or missing information. A qualified virtual claims assistant can track down those pending claims and follow through until they’re finalized. They’ll contact claimants and providers to clear up delays or ensure the next steps.
Claim processing outsourcing ensures no claim gets forgotten or buried under busy schedules. This kind of detail-oriented attention can speed up approvals and payments dramatically. With pending claims handled, you can focus on building your business instead of chasing old claims.
10. Custom Reporting and Analytics
Understanding trends in your claims can help improve your processes over time. A virtual verifier assistant can pull data, find patterns, and create reports tailored to your needs. This can help identify where claim delays happen most or highlight accounts that need attention.
Delegating these insights to a virtual claims assistant saves you hours of manual reporting time. With meaningful data at your fingertips, you can make better decisions for your company. Reports from a qualified assistant help you spot opportunities to save time and money in managing claims.
What Types of Claims Can a Virtual Assistant Handle?
Handling claims can be time-consuming and overwhelming for business owners. Virtual assistants (VAs) are here to make this process smoother and more efficient. They can take on a wide range of claims-related tasks, freeing up your time and ensuring nothing slips through the cracks.
Whether you run a small business or manage a large team, knowing what tasks a VA can handle is essential to solving your administrative headaches. Below are the specific types of claims they can help with and how this support can benefit your business.
1. Insurance Claims Processing
Virtual assistants can manage insurance claims from start to finish, allowing you to focus on what truly matters in your business. They gather and organize all documentation, such as invoices or receipts, needed to file claims accurately.
You won’t have to worry about missing paperwork because they double-check everything before submission. VAs stay on top of deadlines to ensure claims are filed promptly, so you don’t risk losing reimbursement. They can also handle communication with insurance companies, saving you the headache of being on hold. When questions or disputes arise, your VA can quickly liaise with agents to resolve them.
By taking this task off your plate, you avoid delays and get more value from your insurance provider. Their expertise in this area can turn a frustrating process into one you never have to think twice about.
2. Customer Refund or Return Claims
Processing refunds and return requests is another task virtual assistants excel at. They can communicate directly with customers to gather necessary information like receipts or proof of purchase. This ensures the process moves smoothly and eliminates any confusion or complaints. Your VA can coordinate refunds through your payment systems or communicate with your finance department.
They can also update your inventory or issue replacement products when needed, ensuring accuracy across all platforms. By managing these requests, virtual assistants help enhance customer satisfaction and protect your business’s reputation. They work to resolve issues quickly so customers feel valued and looked after.
When your clients see how efficiently refunds and returns are handled, it can boost trust in your brand.
3. Vendor Dispute Claims
Issues with vendors are inevitable, but a virtual assistant can make resolving them far less stressful. They can document the problem, gather purchase records, and draft clear, professional communication to settle disputes. Instead of you spending hours going back and forth, your VA can stay on top of the situation and push for resolutions.
They tackle all the details from delayed deliveries to quality issues while keeping you informed. They can also negotiate settlements, such as discounts or replacements, so you don’t lose valuable business deals. If legal action becomes necessary, your VA can assist in gathering evidence and helping you prepare.
Their ability to stay organized and calm under pressure ensures that disputes cause minimal disruption to your operations. Having someone dedicated to vendor claims means you can maintain strong working relationships while avoiding unnecessary stress.
4. Warranty Claims
Virtual assistants can handle warranty claims on your behalf when a product your business relies on malfunctions or breaks down. They will ensure all warranty documents are securely stored and up to date, so there’s no scrambling to find details when something needs fixing.
Your VA can file the claim with the manufacturer or retailer, ensuring all necessary forms are completed correctly. They can also track the claim and follow up to ensure it’s resolved without delays. They’ll coordinate the entire process if a replacement or repair is needed, keeping you updated at every step.
Additionally, they can keep a schedule for expiring warranties, so you never miss out on coverage you’ve already paid for. This kind of proactive management saves money and avoids downtime caused by failed equipment. With a VA handling warranty claims, you’ll always stay one step ahead.
5. Medical Claims
Navigating medical claims can be confusing, but a virtual assistant can simplify this task for you or your business. They can collect all medical bills, insurance information, and other necessary documents to prepare the claim.
They’ll ensure that claims are submitted correctly, avoiding mistakes that could lead to delays or rejections. Your VA can monitor the claim’s status and follow up with healthcare providers or insurance representatives for updates. If there’s a denial, they’ll investigate the reason and help appeal the decision.
Managing these administrative burdens helps you avoid costly errors while ensuring timely reimbursements. Whether it’s for employee benefits or personal needs, a VA’s attention to detail can make the process stress-free. You’ll also have peace of mind knowing these sensitive claims are handled discreetly and professionally.
6. Freight Damage Claims
When goods arrive damaged or fail to arrive altogether, virtual assistants can quickly take action on freight claims. They’ll start by gathering essential information like bills of lading, photos of damage, and proof of delivery.
This thorough documentation can speed up the claims process and improve your chances of reimbursement. Once the claim is submitted, your VA will continue to follow up with the carrier to ensure a timely resolution. They’ll relay updates to you, so you’re never left in the dark about the progress.
Their help can minimize losses and recover funds that might otherwise be written off. These efforts can save you significant time, especially if your business frequently ships goods. Instead of letting freight issues eat into your profits, trust a VA to keep things moving smoothly.
7. Expense Reimbursement Claims
Tracking and submitting expense reimbursements can be time-consuming, but this is another area where virtual assistants shine. They can collect receipts and expense reports from employees, organize them, and ensure submissions meet company policies.
Your VA can prepare reimbursement claims on your behalf and submit them through your preferred system or process. They’ll keep an eye on deadlines, so reimbursements are processed without unnecessary delays. Monitoring these claims also helps identify errors or inconsistencies, which can protect your business from financial waste. If an issue arises, they’ll handle the back-and-forth with HR or finance departments, saving you the hassle.
With VA managing reimbursement, you’ll have a streamlined approach that keeps your team happy and your books in order.
8. Small Claims or Legal Disputes Assistance
Virtual assistants can play a supportive role in handling small claims or legal disputes for your business. They help by organizing all relevant documentation, including contracts, communications, and payment records. This organized approach makes it easier to present a strong case, whether you’re seeking compensation or defending a claim.
Your VA can also assist with preparing court paperwork or scheduling meetings with legal advisors. While they don’t offer legal advice, their administrative skills ensure nothing is missed in your case preparation. They can track deadlines and manage correspondence, so you remain on top of the process.
Their structure and attention to detail allow you to focus on core business matters rather than getting bogged down in legalities. By having this reliable support, you can handle disputes confidently and efficiently.
How Do Claims Management Virtual Assistants Ensure Compliance?
1. Familiarity with Regulations
Claims management virtual assistant stays current with federal, state, and industry-specific insurance claims processing regulations.
They ensure all submissions comply with regulations, working closely with medical billing assistants and virtual processors.
Their expertise minimizes compliance risks and supports practices adhering to legal standards efficiently.
Regulatory updates are integrated into daily claims management tasks, ensuring seamless compliance.
This familiarity helps organizations avoid penalties while maintaining operational integrity.
2. Error-Proof Submission
Assistants skilled in medical billing VA tasks review claims meticulously before submission, avoiding missteps that could trigger rejections.
Using tools like virtual medical billing systems ensures error-free handling of claim details at every step.
Virtual verifier assistants double-check submissions for verification, adding another layer of scrutiny and accuracy.
Ensuring claims are complete and correctly submitted decreases the chances of compliance breaches.
Comprehensive reviews ensure all claims meet insurer and regulatory requirements consistently.
3. Compliance Documentation
Virtual assistants manage documentation to ensure all claim-related files are well-organized and accessible for audits or reviews.
Proper documentation includes proof of verification, regulatory updates, and detailed claims records maintained efficiently.
Virtual insurance verification assistants ensure files are in order, preventing compliance issues during inspections.
Compliance-focused records contribute to smoother operations while offering clarity and confidence during external reviews.
Strong documentation practices protect the reputation and financial stability of your practice.
4. Collaboration with Experts
Working closely with third parties like medical billing virtual assistants ensures compliance across complex claims processes.
Collaborating between virtual processor assistants and insurance providers fosters smoother and faster compliance-ready document submissions.
Their combined expertise reduces the likelihood of denial or returned claims due to insufficient compliance measures.
Professional partnerships maintain consistency with regulatory guidelines while improving overall submissions.
This collaborative approach effectively aligns practices with broader industry requirements.
5. Risk Mitigation Strategies
Virtual assistants implement proactive strategies to detect and address compliance risks early.
Experienced assistants in claims management roles identify patterns and potential red flags that could result in regulatory violations.
From medical billing in VA settings to broader virtual assistant roles, they strengthen compliance frameworks substantially.
Reduced risks mean smoother audits and safer operations for healthcare and insurance organizations.
Ongoing monitoring ensures lasting compliance without interruptions to regular workflows.
Why Consider Outsourcing Claims Management Virtual Assistant Tasks?
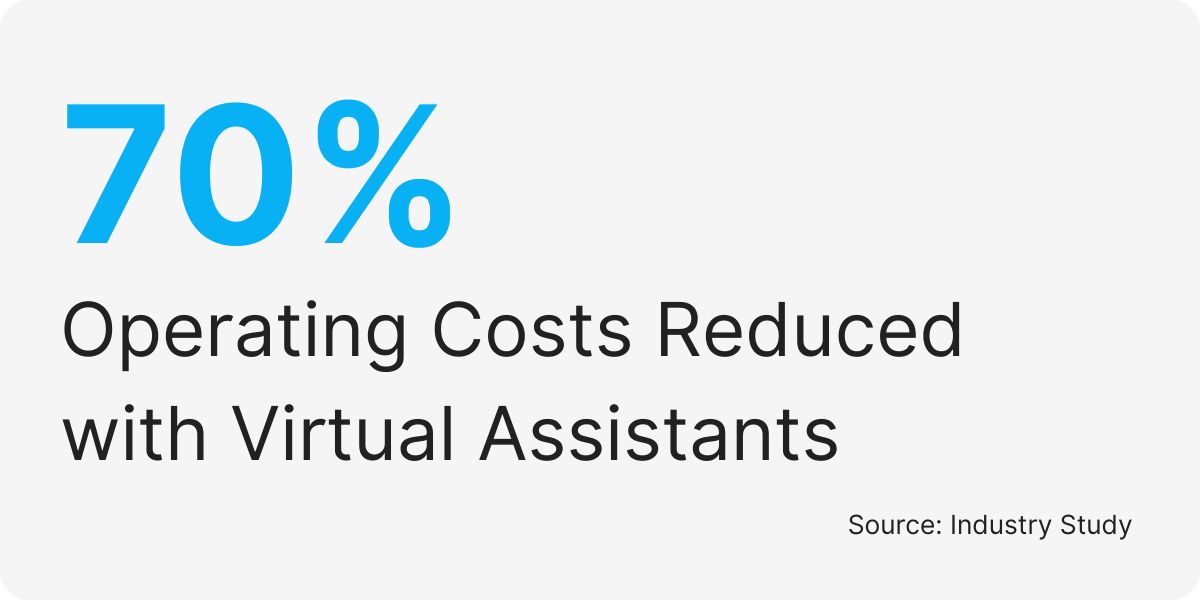
1. Enhance Flexibility
Outsourcing to a claims management virtual assistant provides Flexibility, allowing practices to adjust services based on demand.
Virtual assistant US timezone availability ensures tasks are completed within your required timelines, regardless of location.
The ability to hire specialized roles, like ADHD assistants or virtual insurance assistants, ensures tailored and reliable administrative support.
Outsourced virtual assistant services are scalable, effectively accommodating fluctuating workloads during peak periods.
2. Improve Efficiency
Outsourcing to virtual assistants streamlines workflows, and efficiency claims are processed accurately and quickly.
Assistants utilize tools for virtual medical billing and verification to complete tasks faster than traditional in-house teams.
Hiring skilled Medva virtual assistants increases practice productivity by reducing delays and speeding up reimbursements.
This Efficiency allows healthcare providers to focus on core operations and achieve administrative efficiency.
Enhanced workflows promote long-term success for both the organization and patient satisfaction.
3. Minimize Costs
Outsourcing claims management tasks to a virtual assistant eliminates expenses associated with hiring full-time staff.
Virtual assistants provide the same specialized expertise at a fraction of the cost, making them an ideal choice.
Roles such as virtual processors and medical billing virtual assistants offer professional solutions without straining your budget.
By outsourcing, practices can allocate saved resources to improve other areas like patient care and technology upgrades.
Cost-effective assistance ensures financial stability while maintaining high-quality claims processing services.
This adaptability guarantees consistent claims management in a dynamic healthcare landscape.
4. Reduce Errors
Errors in insurance claims can cause delays and financial losses, highlighting the importance of outsourcing to high-accuracy virtual assistants.
Experienced medical billing assistants review claims for compliance and accuracy, preventing rejections and delayed reimbursements.
With reliable virtual verifier assistants, every detail is checked thoroughly, ensuring no error affects your claims.
Additionally, virtual insurance assistants maintain compliance with updated industry standards, minimizing risks of penalties.
Reduced errors enhance your practice’s Efficiency for patients and insurance providers alike.
5. Increase Focus on Patients
Administrative burdens often take employees from delivering personalized patient care, making outsourcing a vital solution.
A virtual assistant manages time-consuming tasks, so internal teams can spend more time addressing patient needs.
This reallocation of responsibilities improves the overall patient experience while maintaining operational Efficiency and aligns with risk management quotes.
Outsourcing services like virtual medical billing ensures efficiency management never compromises the quality of care.
Enhanced focus on patient care differentiates your practice and attracts loyalty from patients in highly competitive industries.
Can A Claims VA Manager Handle International Claims?
Yes, a claims management virtual assistant can efficiently manage international claims.
With expertise in handling diverse claim types, they ensure accurate processing, even when dealing with complex global regulations.
Stealth Agents offers skilled virtual verifiers and virtual processor assistants trained to navigate international claim requirements.
These professionals can handle tasks such as verifying coverage, submitting claims, and following up on payments across different countries.
For medical practices, a medical billing assistant within this role can also manage international medical claims, staying compliant with varying healthcare laws.
Using advanced tools and knowledge, virtual assistants can reduce errors and save time for businesses managing cross-border claims.
This makes them an invaluable resource for companies operating in international markets.
Takeaways
Claims management virtual assistants simplify complex administrative processes vital to insurance and healthcare organizations.
Stealth Agents trained professional roles like medical billing assistants and virtual insurance verification assistants.
Flexible schedules, such as virtual assistant US time zones, ensure tasks are completed on time while adapting to organizational needs.
Female virtual assistants, ADHD assistants, and others cater to diverse requirements, enabling personalized and efficient solutions.
Enhanced compliance through virtual verifier assistants safeguards against penalties and regulatory issues, protecting your practice’s reputation. By outsourcing claims management tasks, healthcare providers achieve higher Efficiency, affordability, and accuracy.
Choose Stealth Agents for seamless claims workflow management and professional support tailored to your organization
Frequently Asked Questions
How much does a claims management virtual assistant cost per hour?
The cost of a claims management virtual assistant can vary based on their level of experience and skillset. Assistants with extensive experience in claims processing may have a higher rate but can often provide greater accuracy and efficiency. Most virtual assistant companies provide transparent pricing with no hidden fees.
What qualifications should I look for when hiring a claims management virtual assistant?
Look for assistants with experience in medical coding, insurance processing, or claims management. They should know how to use claims software like Epic or Cerner, understand CPT/ICD codes, and follow HIPAA rules. Certifications from groups like AAPC or AHIMA are a plus. Good communication skills and attention to detail are also important.
Can a claims management virtual assistant work with my existing claims software?
Yes, experienced assistants can use most claims management systems like Epic, Cerner, NextGen, and AdvancedMD. They are often trained on multiple platforms and can quickly learn your specific software. Many companies also provide ongoing training to keep assistants updated on new tools and features.
What security measures protect sensitive claim data when working with virtual assistants?
Professional companies use strong security measures like encrypted communication, secure VPNs, and HIPAA-compliant data handling. They monitor workstations, require signed confidentiality agreements, and perform regular security checks. Look for companies with SOC 2 compliance and clear data protection policies to keep your claims information safe.
How quickly can a claims management virtual assistant start working on my claims?
Most companies can match you with a qualified assistant in 5-10 business days. This includes consultation, skills checks, and onboarding. Once matched, the assistant may need 1-2 days to set up systems and learn your processes. Some companies offer faster placements for urgent needs.
Do claims management virtual assistants provide their own equipment and software licenses?
Most companies provide the necessary equipment, like computers and secure internet, as well as basic software. However, you may need to provide licenses for specialized claims software. Reputable companies will explain what they provide and what you need to supply during the consultation.
Can a claims management virtual assistant handle claims for multiple insurance providers simultaneously?
Yes, experienced assistants can work with multiple insurance providers like Medicare, Medicaid, Blue Cross Blue Shield, and Aetna. They understand the different forms, rules, and timelines for each provider, making it easier to manage claims for a variety of clients.
What happens if my claims management virtual assistant makes an error or needs replacement?
Good companies offer guarantees and will replace an assistant if they don’t meet your expectations. They also provide error correction services and have backup assistants ready to step in if needed. Look for companies with clear policies for handling mistakes and replacements.
Are claims management virtual assistants available during my business hours in different time zones?
Yes, many assistants can work during your business hours, no matter where they are located. Some companies offer assistants in multiple time zones or provide 24/7 support for urgent claims. This flexibility ensures you get help when you need it.
What training do claims management virtual assistants receive on healthcare regulations and compliance?
Claims management assistants are trained in HIPAA rules, healthcare regulations, and best practices. They also get regular updates on new laws, proper documentation, and privacy rules. Many have certifications in medical billing and coding and take refresher courses to stay current with industry changes.